Executive Summary:
This study examines how homecare services relate to healthcare use and costs among children with medical complexity (CMC) enrolled in North Carolina Medicaid. CMC are a small but high-need pediatric group with serious chronic conditions, functional limitations, and heavy reliance on coordinated care. Their families face substantial caregiver burden, and many health systems are exploring home-based models of care as a way to improve coordination while reducing costly hospital use. However, quantitative evidence on how homecare interacts with emergency department (ER) and inpatient (IP) utilization in Medicaid populations remains limited.
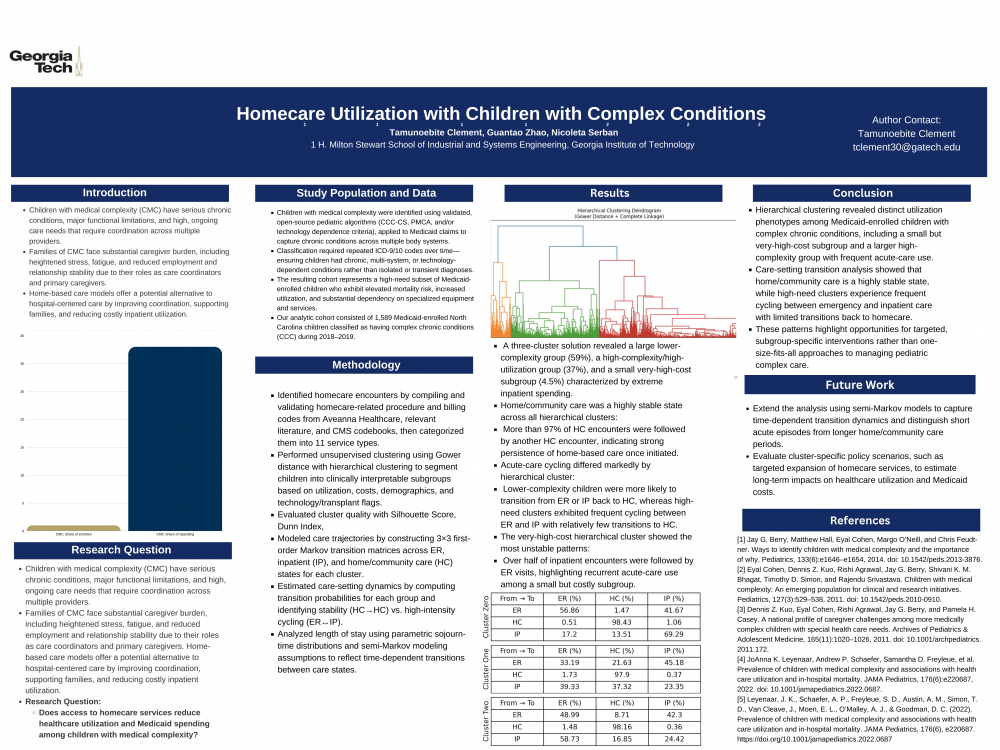
Using 2018–2019 North Carolina Medicaid claims, the study first classifies children into clinically meaningful subgroups. Mixed-type variables—demographics, clinical indicators, utilization counts, and ER/IP costs—are clustered using Gower distance with hierarchical clustering and Partitioning Around Medoids (PAM). After trimming extreme cost outliers, hierarchical k=3k=3k=3 and PAM k=2k=2k=2 solutions provide the best balance of separation and interpretability (Silhouette ≈ 0.60; Dunn ≈ 0.20–0.33), with high agreement between methods (ARI = 0.89). The resulting clusters reveal a gradient from a large, lower-complexity, lower-cost group to a small very-high-cost group and a sizable high-complexity, high-utilization group.
To understand care trajectories, the paper constructs cluster-specific transition matrices across three states: ER, IP, and home/community care (HC). HC is highly stable (>97% of HC encounters lead to HC across clusters), while high-need clusters show frequent cycling between ER and IP and relatively few transitions back to HC. In contrast, lower-need clusters are more likely to move from acute care back into HC, consistent with more stable and potentially better-managed care patterns.
The findings suggest that a targeted expansion of homecare and community-based supports for high-need clusters could help shift trajectories away from recurrent acute care use and reduce overall costs, though causal effects of homecare cannot be established from these analyses alone. The report outlines semi-Markov modeling as a key next step to incorporate state duration and patient-level covariates, enabling richer policy simulations of how changes in homecare intensity might alter long-term utilization and expenditure for Medicaid-enrolled CMC.
Research Motivation:
Children with medical complexity (CMC) represent a distinct pediatric pop- ulation characterized by serious chronic conditions, significant functional lim- itations, and high healthcare needs requiring ongoing, coordinated care from multiple providers [2, 4]. While operational definitions vary across studies and healthcare systems, CMC consistently demonstrate elevated care requirements that extend beyond typical pediatric healthcare delivery.
The burden of caring for CMC extends substantially beyond direct medical man- agement. Parents of CMC report significantly higher levels of stress, fatigue, and anxiety compared to parents of typically developing children, frequently as- suming concurrent roles as care coordinators, medical advocates, and primary caregivers [3]. These multifaceted responsibilities often result in employment limitations, relationship strain, and caregiver burnout. Effective interventions must therefore address both caregiver burden and quality of life while reducing dependence on resource-intensive hospital-based care.
Home-based care represents a promising alternative care delivery model, trans- ferring essential medical services from institutional settings to the home envi- ronment while preserving care continuity. Evidence suggests this approach may enhance care coordination, provide family support, and decrease costly inpa- tient utilization [1]. However, limited empirical evidence exists regarding the impact of homecare services on healthcare utilization and costs among Medicaid- enrolled CMC. This knowledge gap motivates the central research question: Do homecare services reduce healthcare utilization and costs for children with med- ical complexity enrolled in Medicaid?
Research Objective:
This study evaluates the association between homecare service utilization and healthcare costs among children with medical complexity (CMC) enrolled in Medicaid. Using North Carolina Medicaid claims data from 2018–2019, we employ a multifaceted analytical approach to address heterogeneity and care trajectories. Specifically, we: (1) apply unsupervised clustering algorithms to identify distinct patient subgroups based on demographic, clinical, and utiliza- tion characteristics; (2) implement discrete-time Markov models to estimate transition probabilities between care settings, including homecare, emergency departments, and inpatient facilities; (3) fit parametric distributions to sojourn times (length-of-stay) in each care state; and (4) apply a semi-Markov model to estimate state-dependent transition probabilities and expected healthcare costs. This analysis will provide insights into how homecare utilization patterns relate to overall healthcare costs and acute care use, informing Medicaid policy decisions for CMC populations.
Research Methodology:
Children with CCC are the primary beneficiaries of home care services. To better understand home care utilization among CCC patients, we conducted a detailed study and categorization of homecare services. The identification of homecare-related codes was based on three primary sources: codes provided by our partner Aveanna Healthcare, findings from relevant literature [8-9], and codes independently identified from our CMS database. Once homecare codes were systematically identified and classified into 11 distinct service categories (detailed in Table 4: Homecare Codes), we turned to analyzing patterns of healthcare utilization across the patient population.
To identify clinically meaningful patient subgroups and distinguish high health- care utilizers, we applied two unsupervised clustering approaches suited for heterogeneous claims data: Gower distance–based hierarchical clustering and Partitioning Around Medoids (PAM). As part of preprocessing, we reduced the influence of extreme cost outliers by removing observations with inpatient or ER paid amounts above the 95th percentile, based on boxplot inspection of nu- merical features. We then clustered patients using variables capturing Medicaid healthcare costs (ER and IP paid amounts), utilization counts (number of ER visits, total IP claims), demographics (age, race, gender), and binary clinical flags (present-on-admission status, transplant, technology-related dependence), and computed pairwise dissimilarities using Gower distance to accommodate mixed variable types. Hierarchical clustering used an agglomerative complete- linkage procedure to explore multi-level structure, while PAM served as a com- plementary, outlier-robust medoid-based method appropriate for skewed utiliza- tion data. We evaluated cluster quality using the Silhouette Score and Dunn Index and assessed consistency between methods using the Adjusted Rand In- dex (ARI), with higher values indicating better separation and agreement. To examine care-setting dynamics by utilization phenotype, we constructed cluster-specific first-order transition matrices across three states: emergency room (ER), hospital inpatient (IP), and home/community care (HC). For each child, all encounters were ordered chronologically and adjacent pairs of encoun- ters were treated as transitions from state i to state j. Within each cluster (including a reference group of children not assigned to any cluster, denoted cluster = null), we calculated the proportion of transitions from each origin state that ended in each destination state, yielding a 3×3 matrix of transi- tion probabilities (rows = ER/HC/IP at time t, columns = ER/HC/IP at time t+1). These probabilities are reported as percentages in Table X, with larger off-diagonal entries indicating greater movement between care settings within a cluster
Results:
Clustering performance. Across candidate solutions, hierarchical clustering with k = 3 and PAM with k = 2 achieved the optimal balance between cluster separation and clinical interpretability. The hierarchical k = 3 solution yielded a Silhouette score of 0.60 and Dunn index of 0.25, while the PAM k = 2 solution produced a Silhouette score of 0.60 and Dunn index of 0.20. Although DBSCAN configurations generated comparable or higher Silhouette values, their substan- tially lower Dunn indices indicated poorer cluster separation, and these solu- tions were not pursued further. Agreement between the hierarchical and PAM solutions was high (ARI = 0.89), and UMAP projection of the Gower distance matrix revealed two visually distinct regions corresponding to the PAM clusters. PAM clusters (k = 2). PAM partitioned the cohort into a lower-need group (cluster 1, n = 994, 63.2%) and a higher-need, higher-cost group (cluster 0, n = 580, 36.8%). Compared with cluster 1, children in cluster 0 exhibited greater clinical complexity and resource utilization: more chronic conditions (mean 2.13 vs. 1.29), more inpatient claims (5.19 vs. 3.60), more ER visits (6.9 vs. 5.7), and substantially higher mean Medicaid expenditures for inpatient ($62,346 vs. $34,685) and ER care ($12,448 vs. $8,905).
Hierarchical clusters (k = 3). The hierarchical solution refined this pattern into three clinically distinct subgroups: a large lower-complexity cluster (cluster 0, n = 926, 58.8%), a small very-high-cost cluster (cluster 1, n = 71, 4.5%), and a sizeable high-complexity, high-utilization cluster (cluster 2, n = 577, 36.6%). Cluster 0 was characterized by the fewest conditions (mean 1.26), lowest uti- lization (3.52 inpatient claims; 5.8 ER visits), and lowest mean costs (inpatient: $31,800; ER: $8,823). Cluster 1 demonstrated the highest mean inpatient costs ($72,273) despite only moderately elevated utilization, suggesting intensive or specialized care episodes. Cluster 2 combined the greatest clinical complexity (mean 2.13 conditions) with high utilization (5.2 inpatient claims; 6.9 ER visits) and elevated expenditures (inpatient: $62,460; ER: $12,453). Together, these patterns reveal a clear gradient from lower-need to high-need, high-cost children across the derived clusters.
Care-setting transitions Transition matrices for ER, inpatient (IP), and home/community care (HC) revealed distinct patterns by hierarchical cluster (Table X). Overall, transitions from HC were highly stable across groups, with >97% of HC encounters followed by another HC encounter. Differences emerged in trajectories after acute-care encounters. In the reference group (cluster = null), ER visits were most commonly followed by another ER visit (56.9%) or IP admission (41.7%), and IP stays were likely to be followed by another IP stay (69.3%), indicating persistent use of high-intensity services. Cluster 0 showed more favorable dynamics: after ER encounters, children were less likely to re- turn to the ER (33.2%) and more likely to transition to HC (21.6%), and only 23.4% of IP stays were followed by another IP stay, with 37.3% transitioning to 3 HC. In contrast, cluster 1 exhibited the most unstable patterns, with frequent cycling between IP and ER: 58.7% of IP encounters were followed by ER visits and only 24.4% by another IP stay, while ER encounters were followed by either repeat ER use (49.0%) or IP admission (42.3%). These transition patterns are consistent with the high-need, high-acute-care profile of cluster 1 and the more stable HC-oriented trajectories in cluster 0.
Conclusions and Future Work:
Children with medical complexity enrolled in Medicaid exhibit substantial het- erogeneity in clinical complexity, healthcare utilization, and costs. Unsupervised clustering identified a small subgroup of very high-cost, high-complexity chil- dren and a larger group with more stable, lower-cost patterns. Care-setting transition analysis showed that home/community care is a highly stable state, whereas high-need clusters are characterized by frequent cycling between emer- gency department and inpatient care with relatively few transitions back to home/community care. These findings suggest that targeted expansion of home- care and community-based supports for high-need subgroups may help shift tra- jectories away from recurrent acute care use and reduce overall costs, though formal causal evaluation of homecare interventions remains necessary. A natural extension of this work is the development and estimation of semi- Markov models to more fully capture the timing and duration of care episodes for children with medical complexity. Unlike standard Markov models, which assume that transition probabilities depend only on the current state, semi- Markov models allow transition intensities to depend on the elapsed time spent in a state. This framework is particularly well-suited to distinguishing short, un- stable acute-care episodes from longer, more stable periods in home/community care and to characterizing how the risk of ER or inpatient use evolves over time since discharge.
Future analyses could specify state-dependent sojourn time distributions for home/community care, ER, and inpatient states, and incorporate patient- and cluster-level covariates (e.g., clinical complexity, homecare intensity, technol- ogy dependence) into the transition kernels. This would enable estimation of how increased homecare utilization modifies both the duration of time spent in home/community care and the subsequent risk of acute-care transitions, pro- viding a more mechanistic link between home-based services and downstream utilization.
In addition, semi-Markov models could be used to simulate long-term care tra- jectories and costs under alternative policy scenarios, such as expanded eligi- bility for homecare or targeted interventions for high-need clusters, with com- parisons of expected costs and acute-care use across scenarios offering decision- makers quantitative evidence on the potential impact of enhancing home-based services for Medicaid-enrolled CMC.